Patient Education
Our patient education section is designed to enable you to learn more about dentistry and oral health related topics. The more we educate each patient, the more informed everyone is about their dental health. If there is a topic you want to learn more about that you don't find on our website, please let us know. You will find information ranging from what causes bad breath to how to read x-rays to oral cancer. Please check any of the articles below to go directly to that page.

Toothpaste Ingredients Looking at the label on most toothpaste, it would seem that you need an advanced degree in biochemistry to decipher the ingredient names.Propylene glycol, sodium bicarbonate, sodium pyrophosphate, anhydrous dicalcium phosphate and dioctyl sodium sulfosuccinate are all listed. Are you sure you want to put this stuff in your mouth? Fear not. Here is an explanation of which ingredients do what in various types of toothpaste: Hydrogen Peroxide This is one of the few ingredients actually proven to whiten teeth. It is, in essence, a bleach. H.P. is found in the kits dentists can prescribe to bleach your teeth, as well as in over-the-counter bleaching kits. The American Dental Association advises that you should bleach your teeth only under the recommendation and supervision of your dentist. Sodium Bicarbonate It sounds high-tech, but it's actually nothing more than old-fashioned baking soda. It's function in toothpaste is questioned by the ADA, although some dentists say it can help to remove coffee and food stains from your teeth. It is a mild abrasive, so it scours your teeth, helping to eliminate plaque. And it does make your teeth feel clean and smooth. Other abrasives you'll often find in toothpastes are dicalcium phosphate, kaolin, bentonite, silica and calcium carbonate (chalk). Sodium Pyrophosphate This is the active ingredient normally found in tartar-control toothpaste. It has been shown to prevent the formation of plaque when used regularly. However, once tartar hardens onto your teeth, it can't be removed at home. Only a professional cleaning will get rid of it. Propylene Glycol This is a widely-used humectant - an ingredient that keeps the toothpaste moist, and prevents the solid and liquid ingredients from separating. Other common humectants in toothpaste are sorbitol, pentatol and glycerol. Dioctyl Sodium Sulfosuccinate This is a detergent-type ingredient that causes toothpaste to foam in your mouth. You may also see ingredients such as sodium stearyl fumarate and sodium lauryl sulfate. Some believe that the latter (SLS) induces canker sores in people sensitive to this ingredient. As with any product, if use causes discomfort, stop using it and consult your dentist or doctor. Sodium Saccharin This is the least-expensive sweetener, so it is the one you are most likely to see in most toothpastes. It is 600 times sweeter than table sugar, so only a small amount is used to sweeten your toothpaste. Other common toothpaste sweeteners are aspartame and ammoniated diglyzzherizins. Desensitizing Ingredients These are used in toothpastes specially formulated for sensitive teeth. Strontium chloride and potassium nitrate are the two ingredients recognized by the ADA to reduce discomfort if your teeth are sensitive to hot or cold foods. How do they work? They block the transmission of pain to the nerves in your teeth. They don't work immediately - it takes 4-6 weeks for these ingredients to desensitize your teeth. Triclosan This is an antibacterial agent that was recently approved for use in toothpaste by the FDA. It has been used for years as the active ingredient in antibacterial soaps, lotions, sponges and cutting boards. In toothpaste, triclosan has been clinically proven to fight gingivitis in adults by inhibiting the growth of plaque-causing bacteria. Colgate Total, manufactured and distributed by Colgate-Palmolive Co., is the only toothpaste that currently contains the disinfectant triclosan. Other toothpaste manufacturers are expected to follow suit, but since triclosan is considered a drug, all toothpastes that contain it will have to obtain FDA approval before going on the market.

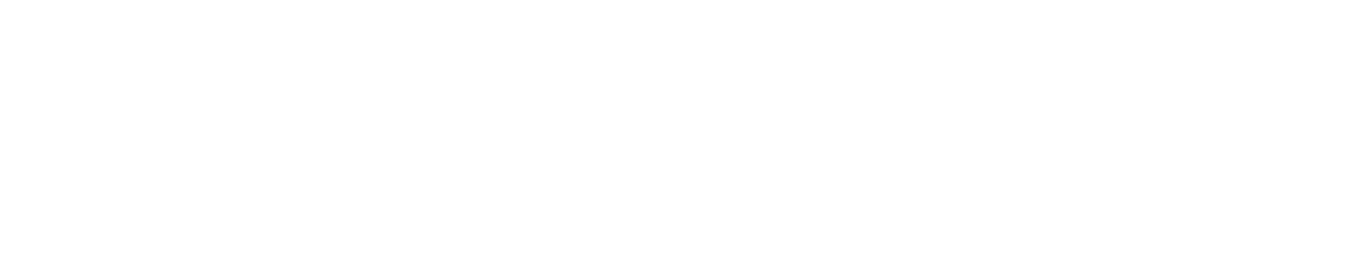
Tooth Sensitivity Do you have or do you know someone who has sensitive teeth? If your answer is yes, you will have a true appreciation for the content of this page. What Is Tooth Sensitivity? It can be defined as a painful reaction in one of more teeth triggered by hot, cold, sweet, or sour foods and drinks. This pain can be sharp, sudden and shoot deep into the nerve endings of your teeth. Apart from a cavity or a missing filling, the most common cause of tooth sensitivity is exposed dentin on the roots of your teeth. Normally, the dentin (the second, more sensitive layer of the tooth) is surrounded and protected by your enamel, cementum (special root covering) and gums. The cause or mechanism of dentinal sensitivity is still not well understood. It is believed that the little tubes that connect the dentin to the nerve or pulp serve as sensory conductors. That sensation may be one of pain. OUCH!! Causes Of Exposed Root Surfaces Which May Result In Dentinal Sensitivity: Brushing too hard - Over a period of time, brushing too hard or using a hard-bristled toothbrush may wear away enamel or cementum and cause the dentin to be exposed. Recession of the gums - Movement of gums away from the tooth due to periodontal disease will expose the root surface. Gum disease - Inflamed and sore gum tissue may also cause sensitivity due to the loss of supporting ligaments which exposes root surface. Other Causes Of Sensitive Teeth: Cracked teeth - Chipped or broken teeth may fill up with bacteria from plaque and enter the pulp causing an inflammatory reaction. Grinding your teeth - Grinding or clenching your teeth may wear down the enamel and expose underlying dentin. Plaque - The presence of plaque on the root surfaces can cause sensitivity. What To Do At Home: Maintain good oral hygiene - Continue to clean all parts of your teeth and mouth thoroughly. Use a soft bristled toothbrush -This will result in less toothbrush abrasion of the tooth surface. Use desensitizing toothpaste - There are many on the market. With regular use you should feel a decreased sensitivity. Try spreading a thin layer on the exposed roots with your finger or a Q-tip before you go to bed. You'll need to find the product that works for you, likely through trial and error. Consider what you eat - If you frequently eat foods high in acids, such as citrus fruits (example: sucking on lemons), they can gradually dissolve the enamel over time, leading to dentin exposure. The citric acids may aggravate the hypersensitivity and initiate a painful reaction. Use fluoridated dental products - As an example, with a daily application of a fluoridated mouthrinse, hypersensitivity usually decreases. Ask us about a daily fluoride rinse for your home use. Professional Care: Ask us what may be used to help reduce sensitivity. Some of the most common treatments are: White fillings to cover exposed root surfaces Fluoride varnish applied to the exposed root surface Dentin sealer applied to the exposed root surface

The Facts About Chewing Tobacco A lot of athletes get hooked before they know the facts about dip and chew. They don't know that spit tobacco: is highly addictive contains nicotine doesn't help performance is not a safe alternative to cigarettes Addiction is one tough opponent. It doesn't take long to get hooked. In fact, you get more nicotine from spit tobacco than from cigarettes. To get unhooked, you have to know what you're up against and you need a game plan. Once you're hooked, it's hard to keep a lid on this. There are no benefits of using spit tobacco. In a Major League Baseball poll, not one player who used dip or chew said that the tobacco improved his game or sharpened his reflexes. Almost all scientists agree that spit tobacco does not improve athletic performance. What's really in it for you? Nicotine (addictive drug) Polonium 210 (nuclear waste) Formaldehyde (embalming fluid) Cancer-Causing Chemicals Radioactive Elements These are just some of the ingredients in dip and chew. Spit tobacco is not a safe alternative to cigarettes. The toxic chemicals can damage your gums. They also can cause cancer. Even if you don't know the harm dip and chew can do, your body does. Cancer is like a bomb! You don't know when it will go off. Up to a certain point, if you quit, your body can heal itself; but the longer you use spit tobacco, the bigger your risk of getting cancer. You don't have to dip for 30 years to get cancer! Quit while you're still ahead of the game. Don't let it be too late. Chewing tobacco and snuff can cause mouth and throat cancer. There are some athletes who have developed mouth cancer after only 6 or 7 years of using spit tobacco. It's hard to cure because it spreads fast. If not caught right away, major surgery is often needed to take out parts of your mouth, jaw, and tongue. Check your mouth often. Look closely at places where you hold the tobacco. See your physician or us right away if you have: a sore that bleeds easily and doesn't heal a lump or thickening anywhere in your mouth or neck soreness or swelling that doesn't go away trouble chewing, swallowing, or moving your tongue or jaw

Oncology Reference Guide to Oral Health Head and Neck Radiation Therapy Pre-Cancer Treatment Oral Health Examination Chemotherapy Oral Complications of Cancer Treatment Blood and Marrow Transplantation Head and Neck Radiation Therapy Patients receiving radiation therapy to the head and neck are at high risk for developing oral complications. Because of the risk of osteonecrosis in irradiated fields, the only opportunity to perform oral surgery may be before radiation treatment begins. Before treatment, we will consider extracting all potentially problem teeth. Before Head and Neck Radiation Therapy See us for a pretreatment oral health examination. Tell us the treatment plan and timetable. Help prevent tooth demineralization and radiation cavities by making sure you have a good oral hygiene program and you have received instruction on fluoride gel application. Allow at least 14 days of healing for any oral surgical procedures. Surgical procedures are contraindicated on irradiated bone, so make sure pre-prosthetic surgery is done before treatment begins. Before Radiation Therapy Make sure you follow the recommended oral hygiene regimen, whether at home or in the hospital. Monitor your jaw for trismus. Check for pain or weakness in masticating muscles in the radiation field. Exercise jaw muscles 3 times a day, opening and closing the mouth as far as possible without pain; repeat 20 times. After Radiation Therapy After mucositis subsides, consult with the oral health team about dentures and other appliances. Patients with friable tissues and xerostomia may never be able to wear them again. Make sure that you follow up with us for fluoride gel/home care compliance and trismus management. Lifelong, daily applications of fluoride gel are needed for patients who are severely xerostomic. Advise against oral surgery on irradiated bone because of the risk of osteonecrosis. Tooth extraction, if unavoidable, should be conservative; use antibiotic coverage and possibly hyperbaric oxygen therapy. For pediatric patients, consult us to monitor irradiated craniofacial and dental structures for abnormal growth and development. Pre-Cancer Treatment Oral Health Examination Objectives Dental decay Periodontal disease Endodontic disease Mucosal lesions Identify and eliminate sources of oral trauma and irritation such as ill-fitting dentures, orthodontic bands, and other appliances. Educate and train patients in preventive oral hygiene: Brush gently after every meal and at bedtime; floss daily. Use special brushing techniques if the mouth is sore. For xerostomia, drink liquids and suck ice chips or sugarless candy. Rinse with 1/4 teaspoon baking soda and 1/8 teaspoon salt in 1 cup warm water solution, followed by a plain water rinse. Keep dentures clean by soaking them daily in antimicrobial solutions and clean water. Remove prostheses if any irritation, mucositis, or ulceration occurs. Evaluate dentition and loss of primary teeth in children. Remove loose primary teeth as well as those expected to exfoliate during treatment. Chemotherapy The oral complications of chemotherapy depend on the drugs used, the dosages, the degree of dental disease, and adjuvant radiation therapy. Before Chemotherapy Schedule an appointment with us for a pretreatment oral health examination. Tell us the treatment plan and timetable. If oral surgery is needed, allow 7 to 10 days of healing before you begin myelosuppressive therapy. In patients with hematologic cancers, we need to check for immunosuppression or thrombocytopenia before any oral procedures. During Chemotherapy Consult with the oral health team to schedule dental treatment. When fever is of unknown origin, consult us to explore a possible oral source of infection. Conduct blood work 24 hours before any dental procedure. Postpone if the platelet count is less than 50,000/mm3, or abnormal clotting factors are present. neutrophil count is less than 1,000/mm3. After Chemotherapy Resume a regular dental recall schedule when chemotherapy is completed and all side effects, including immunosuppression, have resolved. Oral Complications of Cancer Treatment Oral mucositis/stomatitis: Culture infections to identify fungal, bacterial, or viral origin. Work with us on the best control measures. Xerostomia/salivary gland dysfunction: Soften or thin foods with liquid, chew sugarless gum, or suck ice chips and sugar-free hard candies. Suggest using commercial saliva substitute or prescribe a saliva stimulant. Mouth pain: Prescribe topical anesthetics and systemic analgesics. Prescribe antimicrobial agents for known infections. Report oral problems early and to avoid irritating and rough-textured foods. Damaged tooth enamel: To protect enamel, rinse teeth with baking soda and water solution after vomiting. Taste changes: Refer to a dietitian. Specific to Chemotherapy Neurotoxicity: Persistent, deep pain mimics a toothache, but with no dental or mucosal source. Provide analgesics or systemic pain relief. Bleeding from neutropenia: Clean teeth thoroughly with a toothbrush softened in warm water. Avoid flossing the areas that are bleeding but to keep flossing the other teeth. Specific to Radiation Therapy Radiation cavities: Rapid tooth structure breakdown follows radiation therapy, even when the teeth are out of the radiation field. Consult us to prescribe daily fluoride gel applications before treatment begins. Trismus/tissue fibrosis: Do stretching exercises for the jaw to prevent or reduce the severity of fibrosis. Osteonecrosis: Avoid oral surgery that involves irradiated bone. Blood and Marrow Transplantation Most blood and marrow transplant patients develop acute oral complications, especially patients with graft-versus-host disease. Before Transplantation Schedule an appointment with us for a pretreatment oral health examination. Schedule oral surgery at least 7 to 10 days before myelosuppressive therapy begins. Make sure you follow the prescribed oral hygiene regimen and fluoride gel application schedule. Watch for infections on the tongue and oral mucosa. Herpes simplex and Candida albicans are common oral infections. After Transplantation Follow up with us for control of plaque, tooth demineralization, dental cavities, and infection. Delay elective oral procedures for 1 year.

How to Floss Flossing is an essential part of the tooth-cleaning process because it removes plaque from between teeth and at the gumline, where periodontal disease often begins. If you find using floss awkward or difficult, ask us about dental floss holders or interdental cleaning devices that are available. Wind 18" of floss around middle fingers of each hand. Pinch floss between thumbs and index fingers, leaving a 1"- 2" length in between. Use thumbs to direct floss between upper teeth. Keep a 1" - 2" length of floss taut between fingers. Use index fingers to guide floss between contacts of the lower teeth. Gently guide floss between the teeth by using a zig-zag motion. Do not snap floss between your teeth but contour floss around the side of the tooth. Slide floss up and down against the tooth surface and under the gumline. Floss each tooth thoroughly with a clean section of floss.

How to Brush Brushing is an essential part of the tooth-cleaning process. Brushing removes plaque from: the chewing surfaces the cheek and tongue sides of teeth at the gumline, where periodontal disease often begins Most people tend to brush too hard so we strongly advise the use of a soft or electric toothbrush. It is also a good idea to change your toothbrush about every three months. For the back teeth, hold the brush at a 45 degree angle in relation to the gumline (Step 1). Use short, circular strokes as you move the brush at the junction of the gums and teeth. Brush the chewing surfaces of these teeth by holding the brush parallel to the surface of the teeth and brushing back and forth. For the tongue side of the front teeth, hold the brush so that the bristles at the top of the brush contact the gums at a 45 degree angle (Step 2). Again, use short, circular stokes to clean the teeth. For the cheek side, hold the brush from the side at a 45 degree angle and use short, circular strokes (Step 3). You can also brush the surface of your tongue to remove the bacteria and debris that reside on the surface. For flossing instructions, please see How to Floss.

Fluoride Experiment This experiment simulates the protection power of fluoride. What you'll need: 1 bottle of fluoride rinse 2 eggs 1 bottle of white vinegar 3 containers What to do: Pour four inches of fluoride rinse solution into one of the containers and then place an egg in the solution. Let it sit for five minutes. Remove the egg. Pour four inches of vinegar into each of the remaining two containers. Put the egg that has been treated with the fluoride into one container of vinegar and the untreated egg in the other container of vinegar. What will happen: One egg will start to bubble as the vinegar (an acid) starts to attack the minerals in the egg shell. Which egg do you think will start to bubble? The fluoride becomes incorporated into the mineral shell of the egg, thereby protecting it from the acid. Fluoride from toothpaste, mouthwashes, and professional treatments protect the enamel (outer shell) of your teeth in the same manner. Your teeth are constantly under attack from acids in foods, drinks and bacteria naturally occuring in the mouth (plaque).

Dry Mouth What Do I Need To Know About Dry Mouth? Everyone has a dry mouth once in a while--if they are nervous, upset or under stress. But if you have a dry mouth all or most of the time, it can be uncomfortable and can lead to serious health problems. Dry mouth... What is dry mouth? Symptoms include: Why is saliva so important? What causes dry mouth? What can be done about dry mouth? What can I do? Tips for keeping your teeth healthy For more information on Syrgren's Syndrome Dry Mouth... Can cause difficulties in tasting, chewing, swallowing, and speaking Can increase your chance of developing dental decay and other infections in the mouth Can be a sign of certain diseases and conditions Can be caused by certain medications or medical treatments Dry mouth is not a normal part of aging. So if you think you have dry mouth, see your dentist or physician--there are things you can do to get relief. What Is Dry Mouth? Dry mouth is the condition of not having enough saliva, or spit, to keep your mouth wet. Symptoms include: A sticky, dry feeling in the mouth Trouble chewing, swallowing, tasting, or speaking A burning feeling in the mouth A dry feeling in the throat Cracked lips A dry, rough tongue Mouth sores An infection in the mouth Why Is Saliva So Important? Saliva does more than keep the mouth wet. It helps digest food It protects teeth from decay It prevents infection by controlling bacteria and fungi in the mouth It makes it possible for you to chew and swallow Without enough saliva you can develop tooth decay or other infections in the mouth. You also might not get the nutrients you need if you cannot chew and swallow certain foods. What Causes Dry Mouth? People get dry mouth when the glands in the mouth that make saliva are not working properly. Because of this, there might not be enough saliva to keep your mouth wet. There are several reasons why these glands (called salivary glands) might not work right. Side effects of some medicines - More than 488 medicines can cause the salivary glands to make less saliva. Medicines for high blood pressure and depression often cause dry mouth. Disease - Some diseases affect the salivary glands. Sjogren's syndrome, HIV/AIDS, diabetes, and Parkinson's disease can all cause dry mouth. Radiation therapy - The salivary glands can be damaged if they are exposed to radiation during cancer treatment. Chemotherapy - Drugs used to treat cancer can make saliva thicker, causing the mouth to feel dry. Nerve damage - Injury to the head or neck can damage the nerves that tell salivary glands to make saliva. What Can Be Done About Dry Mouth? Dry mouth treatment will depend on what is causing the problem. If you think you have dry mouth, see your dentist or physician. He or she can try to determine what is causing your dry mouth. If your dry mouth is caused by medicine, your physician might change your medicine or adjust the dosage. If your salivary glands are not working right but can still produce some saliva, your physician or dentist might give you a medicine that helps the glands work better. Your physician or dentist might suggest that you use artificial saliva to keep your mouth wet. What Can I Do? Sip water or sugarless drinks often. Avoid drinks with caffeine, such as coffee, tea, and some sodas. Caffeine can dry out the mouth. Sip water or a sugarless drink during meals. This will make chewing and swallowing easier. It may also improve the taste of food. Chew sugarless gum or suck on sugarless hard candy to stimulate saliva flow; citrus, cinnamon or mint-flavored candies are good choices. Don't use tobacco or alcohol. They dry out the mouth. Be aware that spicy or salty foods may cause pain in a dry mouth. Use a humidifier at night. Tips For Keeping Your Teeth Healthy Remember, if you have dry mouth, you need to be extra careful to keep your teeth healthy. Make sure you: Gently brush your teeth at least twice a day. Floss your teeth every day. Use toothpaste with fluoride in it. Most toothpastes sold at grocery and drug stores have fluoride in them. Avoid sticky, sugary foods. If you do eat them, brush immediately afterwards. Visit your dentist for a check-up at least twice a year. Your dentist might give you a special fluoride solution that you can rinse with to help keep your teeth healthy. For more information on Sjogren's Syndrome Sjogren's Syndrome is a major cause of dry mouth. You can get information about dry mouth related to Sjogren's Syndrome from: Sjogren's Syndrome Clinic National Institute of Dental and Craniofacial Research Building 10, Room 1N113 10 Center Drive MSC 1190 Bethesda, MD 20892-1190 Tel: 301-435-8528 Dry Mouth Sjogren's Syndrome Foundation, Inc. Suite 530 8120 Woodmont Avenue Bethesda, MD 20814 Tel: 301-718-0300 or 800-475-6473 www.sjogrens.org

Denture Care Just because you may have dentures does not mean that you can ignore your oral health and hygiene. It is still important to seek regular dental services for evaluating the soft tissues and to examine the denture for proper fit, comfort, and function. Why Should I Clean My Denture Daily? Daily cleaning of your denture is necessary to prevent build-up of plaque, food, calculus (tartar), and stain which can cause: Problems with appearance or esthetics Mouth odor Irritation to the tissues under the denture Infections in the mouth How Do I Keep My Dentures Clean? Rinse the denture under water after meals to remove loose food debris. Brush regularly after each meal, or at least before bed. This removes the plaque and some stains. Brush with water, soap, or a mildly abrasive toothpaste, or denture paste. Scouring powders or other abrasive cleaners should not be used because they scratch the denture. Scratches make the denture more susceptible to collecting debris, plaque and stain. You can use a denture brush or a regular soft toothbrush to clean the denture, but use a separate brush for cleaning any natural teeth you have. Make sure you reach all areas of the denture. The denture can be soaked in a solvent (such as Efferdent, Polident) or a detergent with a chemical action that removes or loosens light stains and deposits. Rinse the denture with water afterwards. Chemical immersions can be done daily or several times a week. Ultrasonic cleaning is done during a dental appointment to remove heavy stain and calculus (tartar). The most effective way to keep your dentures clean is by daily brushing, in combination with soaking the dentures in a chemical solution. Some Helpful Hints: When brushing the appliance do not hold it firmly or with pressure as this can break the denture. Clean the denture over a sink half filled with water and place a towel in the sink to act as a cushion in case the denture should drop. Do not soak or rinse the denture in hot water, this can distort the shape and fit of the denture. Never scrape the denture with sharp instruments in an attempt to remove hard deposits. Instead, take it to a dental professional for them to clean. Make sure to leave your denture out overnight, or out of the mouth for a period of 6 to 8 hours daily. Wearing them at all times without allowing your gums a chance "to breathe" can result in infections of the soft tissues under the denture. When your dentures are not in your mouth, keep them in water or denture solutions. They need to be kept in a wet environment in order to maintain the proper fit Your Gums are Important Too: Not only do your dentures need maintenance, but care also needs to be given to the tissues under your denture. The gums should be cleaned daily with a soft toothbrush or a washcloth. This removes the plaque and debris on the gums. It also massages and stimulates circulation of tissues. Massage your gums by placing the thumb and index finger over the ridge and use a "press-and-release" stroke. Remaining Natural Teeth: It is very important to keep any remaining natural teeth free of plaque. How Do I Know My Dentures No Longer Fit? With age, the jaw bones slowly change. Therefore, dentures may not fit forever. You may need to have your dentures re-adjusted or you may need to have a new denture made. If you encounter any of these problems, let us know. Problems chewing food with dentures Chronic cheek biting Difficulty in speech Red and inflamed tissues Discomfort with wearing the denture Cracked corners of your mouth

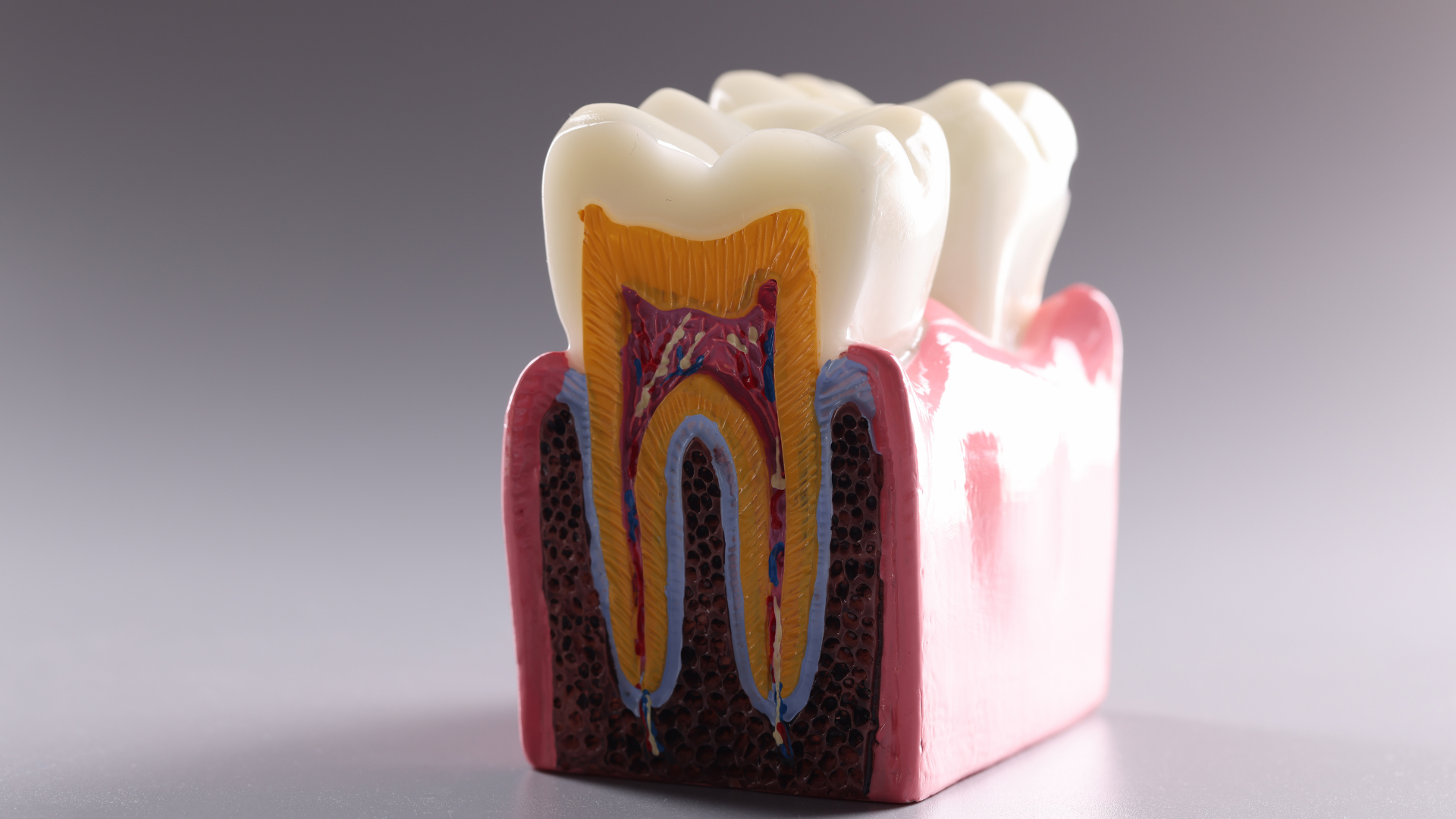
Dental X-Rays - Radiographs What is a Dental X-Ray? The term x-ray is actually referring to the radiation that is used to make the image on the film. The radiograph or picture on the film is the resultant picture that we see. A radiograph is an extremely important diagnostic tool. These pictures show us many things that are not visible by just looking in the mouth. Therefore, radiographs are an essential part of a thorough and complete examination. In order to do a proper checkup, it is important that radiographs are used to help with the visual exam. Without the proper use of both, an inferior examination and inferior treatment will result. Why Do I Need Dental X-Rays? Radiographs show the dental professional things that are not visible to the naked eye. It is also important that old and new radiographs are compared in order to achieve an accurate diagnosis. Who Needs to Have Dental X-Rays? Typically, radiographs need to be taken about every year to 18 months. This is considered the standard of care in dentistry. We prescribe the appropriate type, number and frequency of x-rays based on your needs. Not everyone needs a cleaning and check-up every three months; as well, not every patient needs radiographs as often as the next person. However, some patients may need to have radiographs taken more often. For example, an adult who has had no problems at their last few dental check-ups, and who maintains good oral hygiene at home, may not need check-up x-rays every year. When is it Safe to be Exposed to X-Rays? The ionizing radiation that you receive from one dental x-ray is substantially less that the radiation you receive every day from the sun and stars. Advances in technology have made dental x-rays much safer. Doses of radiation are kept at the lowest practical value to minimize patient exposure. This is done with the use of a long cone position-indicating device, appropriate settings on the machine and using newer, high-speed film. However, it is important to remember that any unnecessary radiation, even a small amount, can damage body tissues. It must be decided if the benefit outweighs the potential risk. Many times a radiograph is necessary to diagnose certain conditions; and therefore, the benefit outweighs the risk . It has been proven that x-rays have a minimal risk on a pregnant woman and her unborn baby. However, radiographs for pregnant women are only taken in an emergency situation. Patients always wear a lead apron and thyroid collar to avoid unnecessary radiation to other parts of the body. This is also the reason that the radiographer leaves the room when taking a radiograph. As the radiographer is receiving no benefit from the exposure, the risk highly outweighs the benefit. There are Three Type of Radiographs that are routinely taken:
Chemo and Your Mouth Chemotherapy and Your Mouth Are You Being Treated With Chemotherapy for Cancer? How Does Chemotherapy Affect the Mouth? What Mouth Problems Does Chemotherapy Cause? Why Should I See a Dentist? When Should I See a Dentist? What Will the Dentist and Dental Hygienist Do? What Can I Do To Keep My Mouth Healthy? Do Children Get Mouth Problems Too? Remember Are You Being Treated With Chemotherapy for Cancer? If so, this information can help you. While chemotherapy helps treat cancer, it can also cause other things to happen in your body called side effects. Some of these problems affect the mouth and could cause you to delay or stop treatment. This information will give you ways to help prevent mouth problems so you'll get the most from your cancer treatment. To help prevent serious problems, see us at least 2 weeks before starting chemotherapy. How Does Chemotherapy Affect the Mouth? Chemotherapy is the use of drugs to treat cancer. These drugs kill cancer cells, but they may also harm normal cells, including cells in the mouth. Side effects include problems with your teeth and gums; the soft, moist lining of your mouth; and the glands that make saliva (spit). It's important to know that side effects in the mouth can be serious. The side effects can hurt and make it hard to eat, talk, and swallow. You are more likely to get an infection, which can be dangerous when you are receiving cancer treatment. If the side effects are bad, you may not be able to keep up with your cancer treatment. Your doctor may need to cut back on your cancer treatment or may even stop it. What Mouth Problems Does Chemotherapy Cause? You may have certain side effects in your mouth from chemotherapy. Another person may have different problems. The problems depend on the chemotherapy drugs and how your body reacts to them. You may have these problems only during treatment or for a short time after treatment ends. Why Should I See a Dentist? You may be surprised that we are important in your cancer treatment. If you see us before chemotherapy begins, you can help prevent serious mouth problems. Side effects often happen because a person's mouth is not healthy before chemotherapy starts. Not all mouth problems can be avoided but the fewer side effects you have, the more likely you will stay on your cancer treatment schedule. It's important for us and your cancer doctor to talk to each other about your cancer treatment. Be sure to give us your cancer doctor's phone number. When Should I See a Dentist? You need to see us at least 2 weeks before chemotherapy begins. If you have already started chemotherapy and you have not seen us, please schedule an appointment as soon as possible. What Will the Dentist and Dental Hygienist Do? Check your teeth. Take x-rays. Take care of mouth problems. Show you how to take care of your mouth to prevent side effects. What Can I Do To Keep My Mouth Healthy? You can do a lot to keep your mouth healthy during chemotherapy. The first step is to see us before you start cancer treatment. Once your treatment starts, it's important to look in your mouth every day for sores or other changes. These tips can help prevent and treat a sore mouth: Keep your mouth moist. Drink a lot of water. Suck ice chips. Use sugarless gum or sugar-free hard candy. Use a saliva substitute to help moisten your mouth. Clean your mouth, tongue, and gums. Brush your teeth, gums, and tongue with an extra-soft toothbrush after every meal and at bedtime. If brushing hurts, soften the bristles in warm water. Use a fluoride toothpaste. Don't use mouthwashes with alcohol in them. Floss your teeth gently every day. If your gums bleed and hurt, avoid the areas that are bleeding or sore, but keep flossing your other teeth. Rinse your mouth several times a day with a solution of 1/4 teaspoon baking soda and 1/8 teaspoon salt in one cup of warm water. Follow with a plain water rinse. Dentures that don't fit well can cause problems. Talk to your cancer doctor or us about your dentures. If Your Mouth Is Sore, Watch What You Eat and Drink. Choose foods that are good for you and easy to chew and swallow. Take small bites of food, chew slowly, and sip liquids with your meals. Eat soft, moist foods such as cooked cereals, mashed potatoes, and scrambled eggs. If you have trouble swallowing, soften your food with gravy, sauces, broth, yogurt, or other liquids. Call your doctor or nurse when your mouth hurts. If the pain continues, talk to your cancer doctor about stronger medicines. Remember To Stay Away From Sharp, crunchy foods, like taco chips, that could scrape or cut your mouth. Food that are hot, spicy, or high in acid, like citrus fruits and juices, which can irritate your mouth. Sugary foods, like candy or soda that could cause cavities. Toothpicks, because they can cut your mouth. All tobacco products. Alcoholic drinks. Do Children Get Mouth Problems Too? Chemotherapy causes other side effects in children, depending on the child's age. Problems with teeth are the most common. Permanent teeth may be slow to come in and may look different from normal teeth. Teeth may fall out. We will check your child's jaws for any growth problems. Before chemotherapy begins, schedule an appointment for us to see your child. We will check your child's mouth carefully and pull loose teeth or those that may become loose during treatment. Ask us what you can do to help your child with mouth care. Remember Visit us before your cancer treatment starts. Take good care of your mouth during treatment. Talk regularly with your cancer doctor and dentist about any mouth problems you have.

Bruxism (Habitual Grinding of Teeth) Have you ever been told that you grind your teeth? Tooth grinding [bruxism] is an oral habit which involves clenching and grinding of the teeth. It is not uncommon in our society. Approximately 50% to 96% of adults experience bruxism and 15% of children acquire this behavior. Most often, this habit goes unnoticed by the person. Bruxism can occur during the day or night. What Causes Bruxism? This condition has no specific cause, but is believed to be a combination of many factors, such as: Emotional stress - personalities characterized as aggressive, controlling, precise, or who have time urgency and achievement compulsion tend to develop bruxism malocclusion (teeth that are not aligned properly) children whose parents brux are more likely to develop this habit than children whose parents do not brux Signs of Bruxism: tooth wear fractures of the teeth and fillings grinding noise noticed by a sleeping partner facial muscle pain and fatigue locking, cracking, and clicking of the jaws headaches tooth mobility sensitive teeth Treatment of Bruxism: We can make you aware of the habit and suggest behavioral therapies to stop the bruxism. Stress reduction and coping techniques can be initiated to reduce the emotional stress you may be experiencing. A removable intra-oral appliance can be made for you called a nightguard or bruxism splint. The mouthguard protects the teeth from the forces of clenching and grinding the teeth together. A mouthguard or nightguard is more practical for treating the night bruxer than for those who have daytime clenching and grinding habits.

Bad Breath (Halitosis) Bad breath (halitosis) can cause embarrassment, create social and psychological barriers, and even affect relationships. Causes The majority of bad breath problems begin in the mouth. Bad breath that is of oral cavity origin can be traced to a sulfur compound produced by bacteria. Dead and dying bacterial cells release this sulfur compound which gives the breath an unpleasant odor. Bacterial plaque and food debris accumulate on the back of the tongue. The tongue's surface is extremely rough and bacteria can accumulate easily in the cracks and crevices. Large amounts of sulfur compounds can be produced in this area, making it a frequent site of origin for bad breath. The tooth attracts bacteria containing plaque and if not cleaned regularly and thoroughly, this can result in large accumulations of bacteria which result in bad breath. People who have periodontitis often experience bad breath because of bacteria accumulating in areas that are not cleaned easily, such as deep pockets around teeth. Fortunately, treatment is very effective for people who have bad breath of mouth origin. Other reasons for bad breath (other than the mouth) are: infections, especially in the sinuses or lungs diabetes mellitus (acetone smell to the breath) kidney failure (can produce a fishy odor) malfunction of the liver disorders of metabolism (foul, fishy odor that comes and goes and may be difficult to diagnose) fasting (when the body is not provided with fuel in the form of food, fat and protein will begin to be broken down; the result is bad odor from the waste products of this metabolism) If your bad breath continues once potential oral health problems have been treated, see your physician to rule out any other causes. Oral Health Treatment Treatment begins with a complete oral examination and health history; you may have an odor-meter test done. This test can accurately measure the volatile sulfur gases and the extent of a halitosis problem. Periodontal disease and /or cavities should be treated and repaired. Oral infections must be eliminated or impacted teeth may need to be removed. Good oral hygiene must be stressed, including cleaning the teeth and tongue. Once the oral infection is treated and cured, mouth rinses and toothpastes may have some effectiveness in managing oral odor. Ask us for a product that may be helpful to you. Bad breath sufferers should be encouraged to seek treatment because of the high success rate in managing the problem.

Acute Necrotizing Ulcerative Gingivitis - Trench Mouth Acute Necrotizing Ulcerative Gingivitis (ANUG), which is also known as trench mouth or Vincent's Stomatitis, is a painful bacterial infection and ulceration of the gums. The term "trench mouth" comes from World War I, when the disorder was common among soldiers. The mouth normally contains a balance of different microorganisms. ANUG occurs when there is an overabundance of normal mouth bacteria resulting in infection of the gums, which develop painful ulcers. Viruses may be involved in allowing the bacteria to overgrow. Symptoms of ANUG include: Painful gums Profuse gum bleeding in response to any pressure or irritation Gums appear reddened and swollen Grayish film on the gums Crater-like ulcers between the teeth Bad breath Foul taste Treating ANUG typically requires antibiotics and dental treatment. Irrigation of the mouth with salt water or peroxide solution often helps to relieve symptoms. Rest, a balanced diet, no smoking, and avoiding hot and spicy foods are also important. Risks include the following: Poor oral hygiene Poor nutrition Throat, tooth or mouth infections Smoking Emotional stress

Acid Experiment This experiment simulates an acid attack on bones (bones are rich with calcium, just like your teeth). What you'll need: 2 clean chicken bones 1 container 1 bottle of white vinegar What to do: Pour several inches of vinegar into the container. Soak the clean chicken bones in the vinegar overnight. What will happen: Check out the bones after they've soaked in the vinegar overnight. Are they softer or harder? How do you think this relates to acid attacking teeth? Be sure to throw the bones away after you have finished.