Oncology Guide
Oncology Reference Guide to Oral Health
- Head and Neck Radiation Therapy
- Pre-Cancer Treatment Oral Health Examination
- Chemotherapy
- Oral Complications of Cancer Treatment
- Blood and Marrow Transplantation
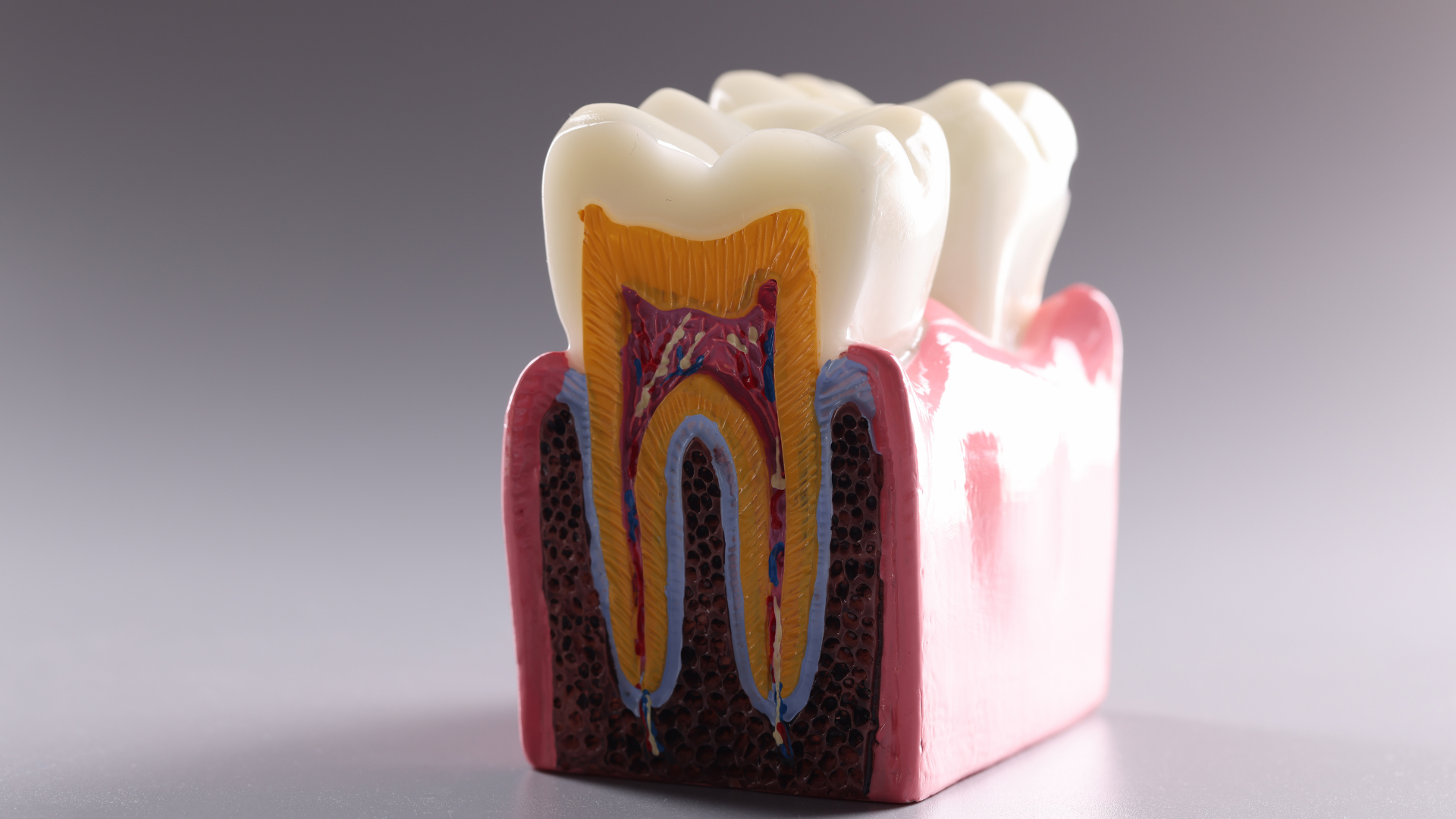
Head and Neck Radiation Therapy
Patients receiving radiation therapy to the head and neck are at high risk for developing oral complications. Because of the risk of osteonecrosis in irradiated fields, the only opportunity to perform oral surgery may be before radiation treatment begins. Before treatment, we will consider extracting all potentially problem teeth.
Before Head and Neck Radiation Therapy
- See us for a pretreatment oral health examination.
- Tell us the treatment plan and timetable.
- Help prevent tooth demineralization and radiation cavities by making sure you have a good oral hygiene program and you have received instruction on fluoride gel application.
- Allow at least 14 days of healing for any oral surgical procedures.
- Surgical procedures are contraindicated on irradiated bone, so make sure pre-prosthetic surgery is done before treatment begins.
Before Radiation Therapy
- Make sure you follow the recommended oral hygiene regimen, whether at home or in the hospital.
- Monitor your jaw for trismus.
- Check for pain or weakness in masticating muscles in the radiation field.
- Exercise jaw muscles 3 times a day, opening and closing the mouth as far as possible without pain; repeat 20 times.
After Radiation Therapy
- After mucositis subsides, consult with the oral health team about dentures and other appliances. Patients with friable tissues and xerostomia may never be able to wear them again.
- Make sure that you follow up with us for fluoride gel/home care compliance and trismus management. Lifelong, daily applications of fluoride gel are needed for patients who are severely xerostomic.
- Advise against oral surgery on irradiated bone because of the risk of osteonecrosis. Tooth extraction, if unavoidable, should be conservative; use antibiotic coverage and possibly hyperbaric oxygen therapy.
- For pediatric patients, consult us to monitor irradiated craniofacial and dental structures for abnormal growth and development.
Pre-Cancer Treatment Oral Health Examination
Objectives
- Dental decay
- Periodontal disease
- Endodontic disease
- Mucosal lesions
Identify and eliminate sources of oral trauma and irritation such as ill-fitting dentures, orthodontic bands, and other appliances.
Educate and train patients in preventive oral hygiene:
- Brush gently after every meal and at bedtime; floss daily.
- Use special brushing techniques if the mouth is sore.
- For xerostomia, drink liquids and suck ice chips or sugarless candy.
- Rinse with 1/4 teaspoon baking soda and 1/8 teaspoon salt in 1 cup warm water solution, followed by a plain water rinse.
- Keep dentures clean by soaking them daily in antimicrobial solutions and clean water.
- Remove prostheses if any irritation, mucositis, or ulceration occurs.
- Evaluate dentition and loss of primary teeth in children. Remove loose primary teeth as well as those expected to exfoliate during treatment.
Chemotherapy
The oral complications of chemotherapy depend on the drugs used, the dosages, the degree of dental disease, and adjuvant radiation therapy.
Before Chemotherapy
- Schedule an appointment with us for a pretreatment oral health examination.
- Tell us the treatment plan and timetable.
- If oral surgery is needed, allow 7 to 10 days of healing before you begin myelosuppressive therapy.
- In patients with hematologic cancers, we need to check for immunosuppression or thrombocytopenia before any oral procedures.
During Chemotherapy
- Consult with the oral health team to schedule dental treatment.
- When fever is of unknown origin, consult us to explore a possible oral source of infection.
- Conduct blood work 24 hours before any dental procedure.
Postpone if the
- platelet count is less than 50,000/mm3, or abnormal clotting factors are present.
- neutrophil count is less than 1,000/mm3.
After Chemotherapy
- Resume a regular dental recall schedule when chemotherapy is completed and all side effects, including immunosuppression, have resolved.
Oral Complications of Cancer Treatment
Oral mucositis/stomatitis: Culture infections to identify fungal, bacterial, or viral origin. Work with us on the best control measures.
- Xerostomia/salivary gland dysfunction: Soften or thin foods with liquid, chew sugarless gum, or suck ice chips and sugar-free hard candies. Suggest using commercial saliva substitute or prescribe a saliva stimulant.
- Mouth pain: Prescribe topical anesthetics and systemic analgesics. Prescribe antimicrobial agents for known infections. Report oral problems early and to avoid irritating and rough-textured foods.
- Damaged tooth enamel: To protect enamel, rinse teeth with baking soda and water solution after vomiting.
- Taste changes: Refer to a dietitian.
Specific to Chemotherapy
- Neurotoxicity: Persistent, deep pain mimics a toothache, but with no dental or mucosal source. Provide analgesics or systemic pain relief.
- Bleeding from neutropenia: Clean teeth thoroughly with a toothbrush softened in warm water. Avoid flossing the areas that are bleeding but to keep flossing the other teeth.
Specific to Radiation Therapy
- Radiation cavities: Rapid tooth structure breakdown follows radiation therapy, even when the teeth are out of the radiation field. Consult us to prescribe daily fluoride gel applications before treatment begins.
- Trismus/tissue fibrosis: Do stretching exercises for the jaw to prevent or reduce the severity of fibrosis.
- Osteonecrosis: Avoid oral surgery that involves irradiated bone.
Blood and Marrow Transplantation
Most blood and marrow transplant patients develop acute oral complications, especially patients with graft-versus-host disease.
Before Transplantation
- Schedule an appointment with us for a pretreatment oral health examination.
- Schedule oral surgery at least 7 to 10 days before myelosuppressive therapy begins.
- Make sure you follow the prescribed oral hygiene regimen and fluoride gel application schedule.
- Watch for infections on the tongue and oral mucosa. Herpes simplex and Candida albicans are common oral infections.
After Transplantation
- Follow up with us for control of plaque, tooth demineralization, dental cavities, and infection.
- Delay elective oral procedures for 1 year.